- Jay Schiff
- 0 Comments
The Main Types of TMS Explained
TMS, or transcranial magnetic stimulation, is a cutting-edge medical treatment that has been used to treat people with depression and other mental health conditions. This procedure employs high-intensity magnetic fields to stimulate nerve cells in the brain and can be applied directly to the head. According to a Harvard study over a third of people who get TMS therapy go into full remission — and more than 30% get some sort of temporary relief from it. Understanding the different types of TMS can help individuals decide if this type of therapy is right for them.
What is transcranial magnetic stimulation?
Transcranial Magnetic Stimulation is a non-intrusive medical procedure that utilizes magnetic fields to trigger and excite nerve cells in the brain.
It is used for the diagnosis and treatment of neurological conditions such as depression, schizophrenia, and Parkinson’s disease.
The history of transcranial magnetic stimulation can be traced back to the late 1800s when a German physician named James Braid came up with the term ‘hypnotism’. He believed that it was possible to create a profound state of relaxation and peace by circulating an electric pulse or current through the brain, and he experimented with this technique on himself and other people.
The first recorded instance of transcranial magnetic stimulation being used for therapeutic purposes took place in 1973 when it was used by Dr. Anthony Barker at the University of Sheffield Medical School to treat depression among patients who had not responded well to conventional treatments such as psychotherapy or drugs.
Some facts about TMS:
- TMS was approved by the FDA in 2008.
- The treatment is covered by most insurance companies — it is a widely accepted form of non-invasive and effective therapy against a multitude of maladies, including OCD, depression, schizophrenia, etc.
- TMS is painless, safe, and fast — it uses magnetic waves to stimulate areas of the brain. This procedure is also very safe as it does not involve any surgery or anesthesia.
- There are multiple fields in which TMS and its tools are being used, including in the mapping of brain functions and neurological studies.
How does Transcranial Magnetic Stimulation Work?
TMS is a highly dynamic and incredibly effective noninvasive method that uses magnetic fields to stimulate the brain. It has been used in neuroscience research for many years, but recent advances in technology have allowed its use as a treatment for various conditions.
The general principle is as follows:
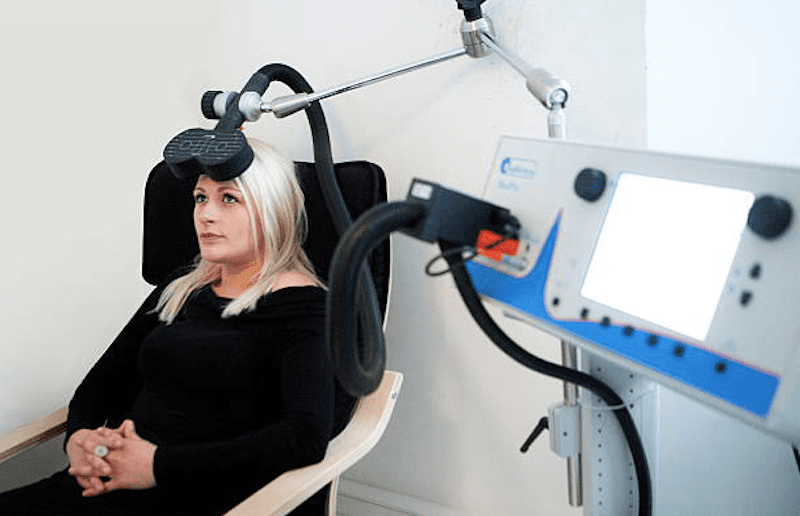
- An electromagnetic coil, placed within a helmet or head cover, is located on the patient’s scalp.
- Then, with the help of software and other apps; as well as a technician, the coil release bursts of magnetic pulses which are responsible for stimulating the nerve cells in different and targeted spots in the brain — each spot directly linked to a neurological condition, for example, depression, mood, executive functions, addictive impulses, etc.
- TMS triggers that region of the brain — lowering its effects.

Benefits Of Transcranial Magnetic Stimulations
There are many benefits of transcranial magnetic stimulation, but one of the most important ones is that it can be used to treat depression. Depression is a debilitating mental disorder and transcranial magnetic stimulation has been proven to be an effective treatment for it.
Other key benefits of transcranial magnetic stimulation include relief from anxiety, bipolar disorder, and insomnia. It can also be used to improve memory, motor skills, and speech.
Transcranial magnetic stimulation has also helped individuals cope with conditions such as addiction, obsessive-compulsive disorder, Tourette syndrome, and Alzheimer’s disease. It can also be used to create artificial memories in the laboratory by stimulating regions of the brain that are involved with memory formation.
Currently, studies are being performed on other associated benefits of TMS therapy including the possibility that it can fight off dementia and mitigate its effects on a diagnosed patient.
There are some risks associated with TMS, including seizures and skin burns — it is not recommended for individuals who have a previous history of seizures or epilepsy because there is a chance that this could happen during or after the session.
Types Of TMS
Right now, transcranial magnetic stimulation therapy is being employed in most fields of neuroscience. Not just to help patients out and alleviate some of the symptoms associated with their disorders or conditions, but as a tool for brain mapping, surgery, and the study of neuro-pathways.
Transcranial magnetic stimulation can be divided into two broad categories/types — those employed for patient care, and those employed for academic research and as a tool for surgery.
RTMS
Repetitive Transcranial Magnetic Stimulation – rTMS – is the most common technique used right now — magnetic fields are applied to the brain to stimulate neurons constantly and repetitively. The stimulation can be targeted at a particular brain region or spread over a larger area. Magnetic fields can penetrate deep into the brain and cause changes in neural activity without any surgery or physical contact with the skull.
There are two types:
- Transcranial direct current stimulation.
- Transcranial alternating current stimulation.
The first one is more common and is used to treat conditions such as depression, drug addiction, and chronic pain. The second type is used to treat brain diseases like Parkinson’s disease, Alzheimer’s disease, and schizophrenia. It can also be used for other purposes such as treating anorexia nervosa.
The treatment is given one day per week for 4-6 weeks and then given less frequently as needed.
It has been shown to be helpful for patients with major depression, obsessive-compulsive disorder, and anxiety disorders such as post-traumatic stress disorder – PTSD.
NTMS
Navigated transcranial magnetic stimulation – nTMS – is a radical and emerging tool in the field of surgery — particularly in the treatment of brain tumors. NTMS is used to create a map of the brain that can then be used as a roadmap during surgery.
STMS
Single-Pulse TMS is a dynamic method being employed in many fields to explore key brain functions and the way they relate to one another.
PpTMS
Paired-Pulse transcranial magnetic stimulation – ppTMS – is one of the most revolutionary methods of TMS available right now — it is fast becoming a popular method to probe both intra-cortical connections – targeted brain region – and inter-cortical connections — the two separate brain regions. It shows promise in the examination of the excitability of inhibitory and excitatory interactions in the human motor cortex.
ITBS
Intermittent Theta-Burst Stimulation – iTBS – is an off-shot of transcranial magnetic stimulation. This type of therapy is potentially faster and more effective in the treatment of depression. iTBS therapy stimulates the cortex by employing a short triple of 50Hz stimulation for only 600 pulses per session. It is a relatively new method of TMS that is being used to treat psychiatric and neurological disorders.
ATMS
Accelerate Transcranial Magnetic Stimulation is a speed-up version of rTMS. The methodology describes a TMS regimen in which a person receives more than one course of treatment per day. In some cases, a person may end up receiving up to ten treatments in a single day for the span of a week. Accelerated Transcranial Magnetic Stimulation is meant to deliver faster relief from depressive and intrusive symptoms — it is mainly employed in dire situations.
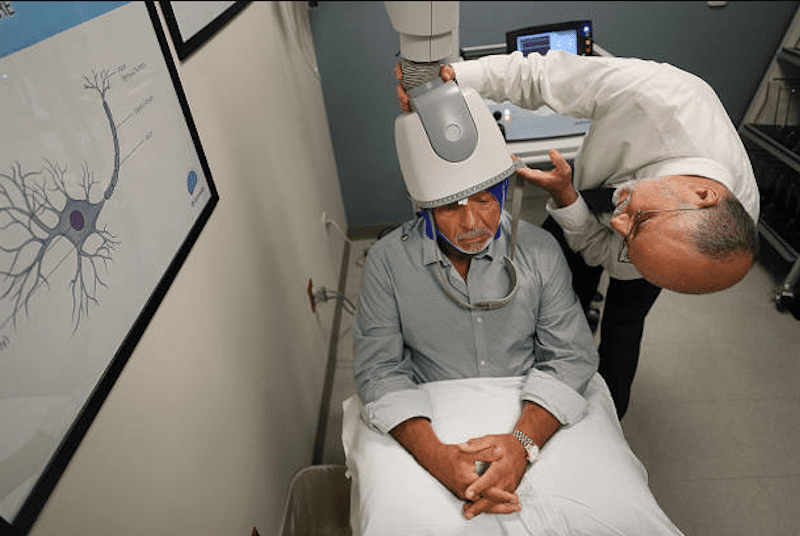
Deep TMS – DTMS
Deep Transcranial Magnetic Stimulation is an upgrade to the standard – 8 TMS treatment. This type of Transcranial Magnetic Stimulation therapy goes further into the brain and penetrates deeper into its makeup by using a unique H-Coil lined device.
DTMS is mostly used to treat other ailments beyond depression, OCD, anxiety, and PTSD.
Choosing The Right Kind Of Transcranial Magnetic Stimulation Therapy
Before undergoing Transcranial Magnetic Stimulation therapy patients may consider the following:
- Getting a physical and psychiatric exam.
- Discussing with your medical provider your interest in TMS and whether it is right for you.
Patients are encouraged to share pertinent facts with their physicians, such as:
- If they are pregnant or are considering it.
- If they have an implant or any metal device inside of them.
- The type of medication they are using.
- If they have a history of epilepsy.
- If they have suffered a previous brain injury.
- If they suffer from frequent and severe headaches.
- Other medical conditions they may want to divulge.
- If they have had prior TMS treatments.
There are a number of different factors which may impact the way TMS works, including:
- The shape and design of the coil itself.
- How many coils are embedded into the TMS device?
- Which part of the brain is being stimulated
- The type of pulse the device uses — whether it is a single or a reputed pulse.
- The intensity and frequency of the stimulation.
- The duration of the therapy itself.
It’s important to talk with your doctor. They will help you understand how TMS works, whether it is something they would prescribe for you, and finally, the type of transcranial magnetic stimulation therapy that is best for you. Each patient is different, and so is each disorder, treatment should be unique and adapt to your needs.